EAHP EU Monitor - 4 October 2017
 The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
You can subscribe to receive the EAHP EU Monitor by email HERE.

EAHP Congress – register as participant and submit your abstract
Gothenburg in Sweden, a beautiful city with an exciting cultural life will be the destination of the 23rd Congress of the European Association of Hospital Pharmacists (EAHP). Hospital pharmacists from all over the world will be gathering from 21st to 23rd March 2018 to attend over 40 educational activities organised under the theme: "Hospital pharmacists – Show us what you can do!".
Submit your abstract by 15th October
Less than 2 weeks left to submit your abstract to the largest hospital pharmacy education event in Europe. The EAHP Scientific Committee encourages all hospital pharmacists, other health care professionals and interested scientists to submit their work for consideration leading to acceptance and display at the upcoming EAHP congress. Submissions need to be provided to EAHP by Sunday 15th October 2017.
Contributors are kindly reminded to carefully read and comply with the guidelines presented on EAHP's website which outline the abstract review process, provide guidance to those submitting abstracts for the first time and list tips on avoiding abstract rejection. Submissions of abstracts from all disciplines of hospital pharmacy or related areas are encouraged, provided that they can be linked to one of the 44 European Statements of Hospital Pharmacy.
Abstracts must be structured and written in five paragraphs (Background, Purpose, Materials and Methods, Results, Conclusions) and they should not exceed the limit of 350 words. The online submission system will guide you through the process. In case you still have questions concerning the abstract submission process, please send an email to abstract[at]eahp[dot]eu
The best abstracts/posters, with regards to aspects like originality, scientific quality and practical applicability, will be awarded with 3 prizes amounting to 750 euro, 500 euro and 250 euro.
More information HERE
Don't forget to register
This Congress continues to provide hospital pharmacists with an exceptional opportunity to meet, network and share expertise and best practice with colleagues while keeping up to date with the latest developments. The educational programme of the 23rd Congress will focus on a variety of topics to showcase the broad range of work that hospital pharmacists carry out.
During the seminars, particular attention will be given on the one hand to medicines shortages, antimicrobial stewardship, advanced therapy medicinal products, clinical trial regulation and ethic committees. On the other hand, aspects of the productive and the effective pharmacist will be explored in sessions on prioritising, process planning and multidisciplinary teams. Workshops will elaborate on the role of the pharmacist in drugs and therapeutics committees; the assessment and clinical importance of pharmacist recommendations; and the check of medication appropriateness.
To ensure that you can benefit from the 3 keynotes, 19 seminars, 3 workshops, 5 Synergy events and the session on Swedish hospital pharmacy, don't forget to register. Early birds will be rewarded with a reduced registration fee that is available until the end of November.
Participation of students and young professionals is encouraged by specific student/young professional rates and a session specifically tailored to student's needs. Aspiring hospital pharmacists will have the chance to learn about an evidence based approach to developing an individual patient care plan.
Register HERE for the 23rd Congress of the EAHP

EUI report – addressing medicines shortages in Europe
Medicines shortage, one of EAHP's key policy priorities, is in the focus of a new report published by the Economist Intelligence Unit (EIU) Healthcare. Addressing medicine shortages in Europe: Taking a concerted approach to drive action on economic, manufacturing and regulatory factors discusses the causes contributing to medicines shortages and provides calls for action on how to address these causes. Both the EAHP report on medicines shortages and expert contributions by EAHP President Joan Peppard were used as resources for the report.
Overall, the report emphasises that the increase in shortages affects patient outcomes, clinicians, manufacturers as well as pharmacists' time and budgets. The drivers of shortages are dependent on many factors. The three main ones, manufacturing, economic and regulatory causes, are considered by the report, in addition to the different views of stakeholders. The actions that are demanded by the report in relation to the prevention and the management of medicines shortages are those that have been identified as being the most promising ones for the different stakeholder groups.
In terms of prevention, the report calls for the improvement of tendering practise and the consideration of specific measures which maintain healthy multi-supplier markets, while for the improvement of shortage management the following actions are demanded:
- Agreement on a common definition of medicines shortages;
- Implementation of an EU early-notification requirement for manufacturers on national level for situations in which medicine shortages are expected;
- Development of a system that ensures transparency about shortages on national level;
- Enhancement of the efficiency of regulatory procedures and the implementation of fast-track processes to mitigate acute medicine shortages;
- Provision of greater flexibility for the delivery of medicines and the movement of packs across boarders during shortage periods.
A key factor to mitigate shortages that was highlighted by the European Shortage Research Network – an initiative funded by European Cooperation in Science and Technology (COST) – is communication between the different stakeholders. The COST Action which is led by EAHP Scientific Committee member Prof Helena Jenzer brings together different stakeholders to address supply problems to patients. The main aim of the initiative over the next three years is to understand the steps needed to mitigate the problem of medicine shortages.
Read the full report HERE
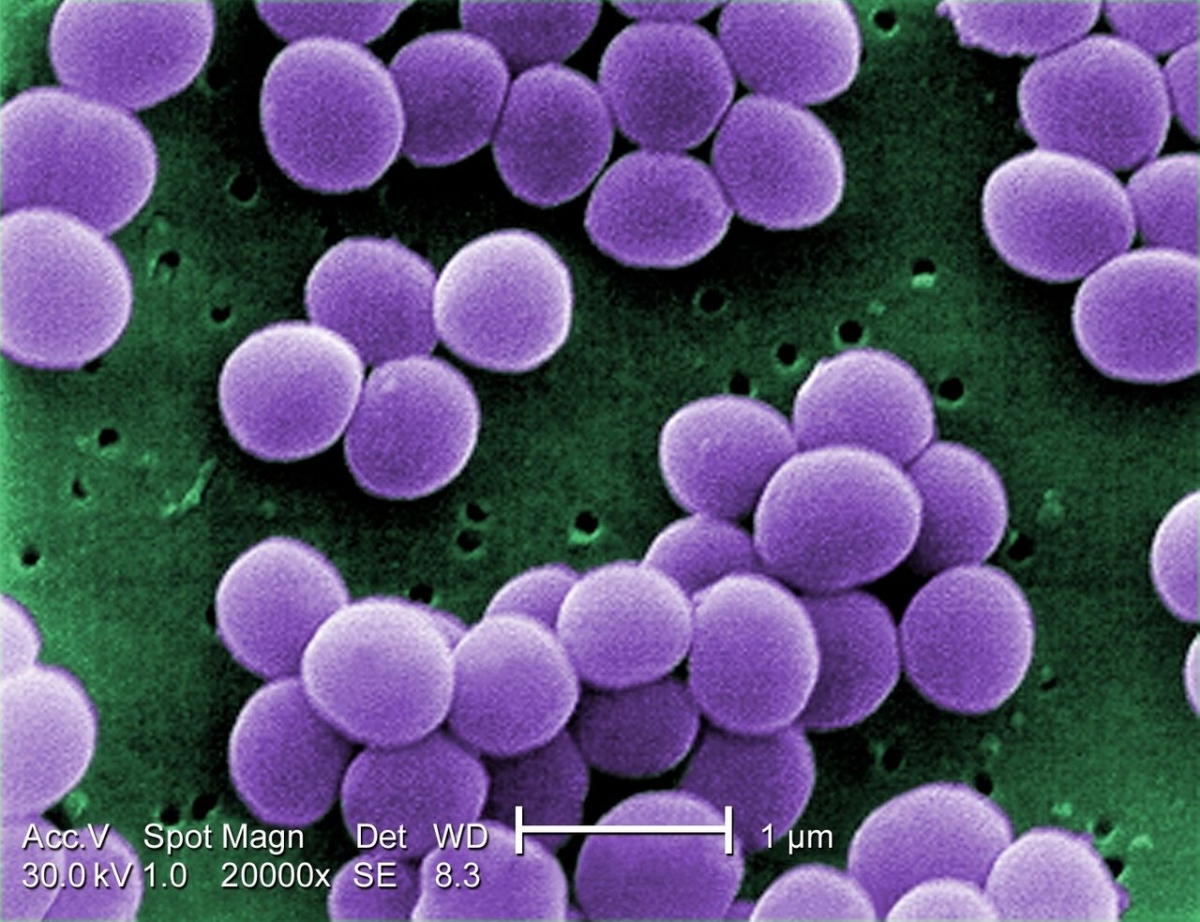
AMR – Antibacterial clinical development pipeline
The World Health Organisation (WHO) released a report that provides an overview on the antibacterial agents in clinical development. It is a follow up action related to the list of priority antibiotic resistance pathogens that was drawn up as part of WHO's Global Action Plan on Antimicrobial Resistance. The report shows a serious lack of new antibiotics, since most of the drugs currently in the clinical pipeline are modifications of existing classes of antibiotics and are thus short-term solutions.
The analysis focused on 62 antibacterial products (51 antibiotics and 11 biologicals) that were as of May 2017 in phase I-III of clinical development and had not yet received a market authorisation for human use. In addition, to classifying the antibacterial products by type, pathogen category, phase of clinical development, and expected activity against priority pathogens, the report also analysed their innovativeness. Only 8 out of the 33 antibiotics that are being developed for priority pathogens fulfilled at least one of the four criteria that were used to assess innovativeness. These criteria include (1) absence of cross-resistance to existing antibiotics, (2) new chemical class, (3) new target and (4) new mechanism of action.
Overall, the report shows that the antibacterial agents currently in clinical development are insufficient to mitigate the threat of antimicrobial resistance. Consequently, more investment is needed in basic science, drug discovery and clinical development. Furthermore, the report calls for more innovative products as these are required against pathogens with no cross- or co-resistance to existing classes.
In addition, to the presentation of the findings the report also highlights the important role of antimicrobial stewardship. The development of new antibiotics is not sufficient to mitigate the threat of antimicrobial resistance, wherefore it needs to go hand in hand with infection prevention and control activities. As outlined in EAHP's position paper on antimicrobial resistance activities fostering the appropriate use of existing and future antibiotics should be undertaken by stewardship teams in which also hospital pharmacists are involved.
Read the full WHO report HERE
A summary of the data is available HERE
Stay tuned for more information on the upcoming European Antibiotic Awareness Day that will be supported by EAHP as well as on the new hospital toolkit that will be released by the European Centre for Disease Prevention and Control (ECDC) shortly.
UGPx – Implementing Pharmacogenomics in Europe
![]()
The Ubiquitous Pharmacogenomics (U-PGx) project, which is funded by the European Union's Horizon 2020 grant, aims at implementing pharmacogenomics in seven EU sites/countries and evaluating patient benefit and cost-effectiveness using a randomized clinical trial design. Overall, the project seeks to address major challenges and obstacles for the implementation of pharmacogenomics (PGx) testing in patient care by taking into account the diversity of health systems and citizens in Europe.
Pharmacogenomics, the study of genetic variability affecting an individual's response to a drug, plays the central role in this project. Its use allows personalized medicine and reduction in 'trial and error' prescribing leading to more efficacious, safer and cost-effective drug therapy. However, despite the advances made in PGx and the availability of PGx tests, application remains very limited.
U-PGx will specifically investigate if the emerging approach of pre-emptive genotyping of an entire panel of important PGx markers is cost-effective and results in a better outcome for patients. With the pre-emptive PGx testing approach data on multiple important pharmacogenes are collected prospectively and embedded into the patients' electronic record. Typically, it alerts prescribers and pharmacists through electronic clinical decision support systems when a drug is ordered or dispensed for a patient with an at-risk genotype. The new model of personalised medicine through pre-emptive PGx-testing will be conducted at a large scale in Austria, Greece, Italy, Slovenia, Spain, the Netherlands and the United Kingdom.
To meet this goal, the U-PGx Consortium combines existing pharmacogenomics guidelines and novel health IT solutions. For this study, existing PGx guidelines (84 drug-gene pairs comprising 13 genes) from the Dutch Pharmacogenetics Working Group have been translated into all local languages of the countries involved (from Dutch to English, German, Greek, Slovenian, Spanish, and Italian) by certified professionals. The guidelines will be published as a series in the international high ranked journal Genome Medicine in order to facilitate their use in patient care.
Details about the study and an overview of implementation studies and programs undertaken in the field of pharmacogenomics are available HERE
Find more information about the project HERE
 EJHP: Pharmacotherapy within a learning healthcare system: rationale for the Dutch Santeon Farmadatabase
EJHP: Pharmacotherapy within a learning healthcare system: rationale for the Dutch Santeon Farmadatabase
The online first edition of the European Journal of Hospital Pharmacy (EJHP) has published an original article focusing on monitoring hospital medicine utilisation in real time through a database constructed by a group of hospitals. The study showed that is feasible for to benchmark the positioning of medicines and monitor their impact on clinical outcomes by means of a self-constructed database.
More HERE
--------------------------------------------------------------

Consultations
EMA – Views on reporting of adverse drug reactions
The European Medicines Agency (EMA) has launched a survey to better understand patients' and healthcare professionals' awareness of reporting adverse drug reactions, including for medicines under 'additional monitoring'.
Deadline – 9th October
More information HERE
Public Consultation on Health and Care in the Digital Single Market
The European Commission has launched a public consultation on transformation of health and care in the Digital Single Market. The consultation investigates the need for policy measures that will promote digital innovation for better health and care in Europe and feed into a new Policy Communication to be adopted by the end of 2017. Participation is open to citizens, patient organisations, health and care professionals, public authorities, researchers, industries, investors and users of digital health tools.
Deadline – 12th October
More information HERE
EMA - Guideline on good pharmacovigilance practices (GVP) - Product- or population-specific considerations IV: paediatric population
The European Medicines Agency (EMA) is consulting on the guideline addressing good pharmacovigilance practices specifically targeting the paediatric population which was recently updated. This guidance should be read in conjunction with Title IV of the Paediatric Regulation and its Article 34, Regulation (EC) No 726/2004 and Directive 2001/83/EC.
Deadline – 13th October
More information HERE
EMA – Reflection paper on the pharmaceutical development of medicines for use in the older population
The reflection paper describes aspects that medicines developers may consider when designing medicines for older people, such as selecting appropriate routes of administration and dosage forms, dosing frequency, excipients, container closure systems, devices and technologies, and user instructions in the product information. It is intended to communicate the current status of discussions on the pharmaceutical development of medicines that may be used in the older population.
Deadline – 31st January 2018
More information HERE
![]()
Upcoming events
18th October - Economics vs Health? EU Proportionality Test for Health Professionals - Brussels, Belgium
The Pharmaceutical Group of the European Union (PGEU), the Council of European Dentists (CED), and the Standing Committee of European Doctors (CPME) are organising a discussion in the European Parliament that will focus on the implications of the EU Proportionality Test for Health Professions.
22nd November – Game Changers for better and affordable medicines for Europe - Brussels, Belgium
The 2017 Universal Access and Affordable Medicines Forum of the European Public Health Alliance (EPHA) organised under the auspices of the Bulgarian Health Ministry aims at setting out a positive agenda of actionable policy recommendations to be implemented at the European and national level. The one-day event will provide participants with stimulating and lively discussions on the hottest topics in pharmaceuticals.




