EAHP EU Monitor - 9 February 2018
The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
You can subscribe to receive the EAHP EU Monitor by email HERE.
EAHP: Leadership Training for Implementation Ambassadors
The 1st EAHP Leadership Training for Implementation Ambassadors was held in Brussels on January 27th and was facilitated by Kayhill Management Consultancy. Participants included implementation ambassadors from 26 different EAHP member countries as well as the EAHP Board.
The network of Implementation Ambassadors, in collaboration with National Member Associations of EAHP, are key for moving towards Statement implementation within EAHP member countries. The training consisted of an interactive session where ambassadors were able to learn and practice some of the skills needed to be effective when influencing, communicating and engaging stakeholders. Implementation ambassadors also worked on developing relevant negotiation and influencing skills for approaching national authorities.
The training described the theory and demonstrated the practical application of tools used for leading large-scale change in complex environments. It also helped ambassadors to:
- Demonstrate practical knowledge of effective stakeholder engagement;
- Demonstrate knowledge and application of negotiation & influencing; and,
- Demonstrate knowledge and application of building ambition & purpose to accelerate change. Implementation ambassadors learned relevant negotiation and influencing skills for approaching national authorities and other relevant stakeholders.
In case you want to learn more about the Statement Implementation project, join us in Gothenburg from 21st to 23rd March. During the 23rd Congress of the EAHP, the Statement Implementation team will be waiting for you at Booth 78 to answer all your questions about the Statement Ambassadors, the Self-Assessment Tool and Statement Implementation Learning Collaborative Centres (SILCC) programme.
More on Statements and implementation HERE
Register for the EAHP Congress HERE
 European Commission: Legislative proposal for health technology assessment
European Commission: Legislative proposal for health technology assessment
The European Commission has issued a legislative proposal for health technology assessment (HTA), in order to optimise the use of resources by Member States and reduce the administrative burden for health technology developers. Under the proposal, a pan-European body will be created, funded by the EU budget, which will coordinate national HTA work beyond 2020.
HTA measures the added value of a new health technology compared to existing ones. Examples of health technologies include medicinal products, medical equipment, diagnostic and treatment methods, rehabilitation, and prevention methods.
The proposed Regulation on HTA aims to ensure a better functioning of the internal market, by improving business predictability and reducing the duplication of efforts. It also tries to heighten the human protection level by improving the availability of innovative health technologies for EU patients and promoting the convergence of HTA tools, procedures and methodologies, thus ensuring long-term sustainability of EU HTA cooperation. The scope of the proposal applies to new medicines and certain new medical devices. Four main areas of cooperation
- Joint clinical assessments focusing on the most innovative health technologies with the most potential impact for patients;
- Joint scientific consultations whereby developers can seek advice from HTA authorities;
- Identification of emerging health technologies to identify promising technologies early; and,
- Continuing voluntary cooperation in other areas are mentioned by the proposed Regulation.
The proposal will now be discussed by the European Parliament and the Council of Ministers. After its adoption and entry into force the new rules would be slowly phased-in over a three-year period. On the one hand, this would allow Member States to adapt to the new processes. On the other hand, it would be ensured that the implementation of the Regulation on HTA does not interfere with the implementation of the Regulations on medical devices and in vitro diagnostic medical devices.
Legislative proposal HERE
More about HTA in the EU HERE
Survey: Support post-doctoral research on medication wastage minimisation
Dr Lorna Marie West is currently pursuing a post-doctoral scholarship within the Department of Clinical Pharmacology & Therapeutics at University of Malta under the mentorship of Professor Maria Cordina and in collaboration with Professor Derek Stewart. Her research comprises of several phases exploring and implementing medication wastage minimisation strategies in Malta and European countries.
Her study is part-funded by the REACH HIGH Scholars Programme – Post Doctoral Grants. The grant is part-financed by the European Union, operational Programme II – Cohesion Policy 2014 – 2020 'Investing in human capital to create more opportunities and promote the well-being of society' – European Social Fund.
A questionnaire to identify wastage minimisation laws and policies, as well as current action plans in place targeting medication wastage minimisation, medication storage and disposal amongst European countries will help identify possible successful strategies that minimise medication wastage.
The questionnaire can be completed voluntarily via the online tool Survey Monkey. The study is not anonymous, but information will be kept completely confidential. Names of participants will not appear in any report or publication arising from this study. Only country names will be published. The full findings of the study will be presented at international conferences and submitted for publication in a peer reviewed journal.
Participate in survey HERE before 27th February 2018
Information letter HERE
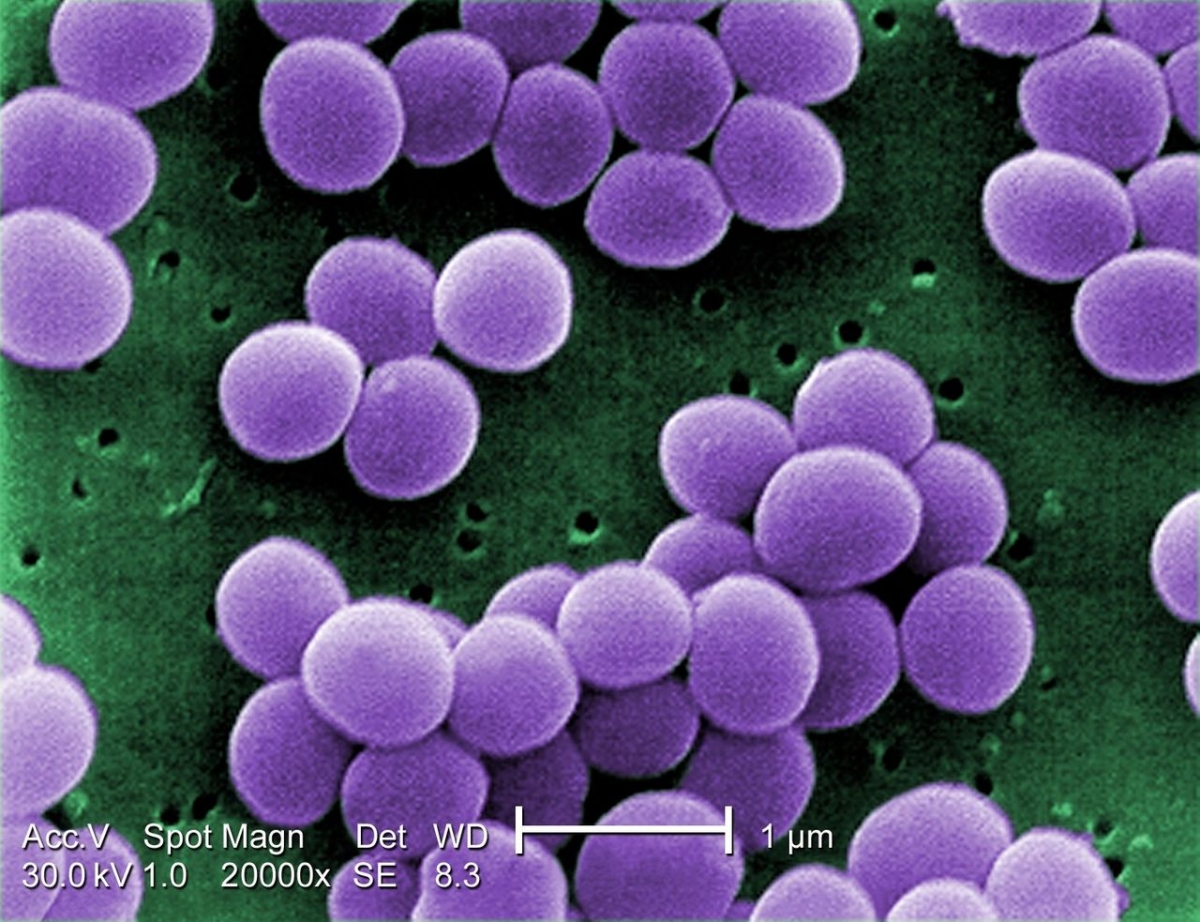 WHO: High levels of antibiotic resistance found worldwide, new data shows
WHO: High levels of antibiotic resistance found worldwide, new data shows
New surveillance data on antibiotic resistance has revealed high levels of resistance to various bacterial infections in both high- and low-income countries. The WHO’s new Global Antimicrobial Surveillance System (GLASS) signals a widespread occurrence of antibiotic resistance among half a million people with suspected bacterial infections across 22 countries. To date, 52 countries are participating in the GLASS (25 high-income, 20 middle-income and 7 low-income countries). There are some obstacles in obtaining data, as some of the participating countries face major challenges in building their national surveillance systems, including a lack of personnel, funds and infrastructure.
However, WHO is supporting more countries to set up national antimicrobial resistance surveillance systems that can produce reliable, meaningful data. GLASS is helping to standardize the way that countries collect data and enable a more complete picture about antimicrobial resistance patterns and trends.
Dr Tedros Adhanom Ghebreyesus, WHO’s Director-General, is aiming to make antimicrobial resistance one of WHO’s top priorities by bringing together experts working on this issue under a newly created strategic initiatives cluster.
More HERE
WHO: Medication without harm challenge
The WHO is working on a global initiative with the aim of reducing severe, avoidable medication-associated harm worldwide by 50% over the next 5 years. Medication errors can result from health worker fatigue, overcrowding, staff shortages, poor training and the wrong information being given to patients.
The Global Patient Safety Challenge on Medication Safety campaign aims to engage key stakeholders in the development and implementation of strategies for medication safety, following the call for action “Know. Check. Ask.” The campaign encourages both patients and health care professionals (for example nurses, physicians, (hospital) pharmacists) to take an active role in ensuring safer medication practices and medication use processes including prescription, preparation, dispensing, administration and monitoring.
The actions planned in the Challenge address four themes: patients and the public; health care professionals; medicines as products; and systems and practices of medication.
This challenge is WHO’s third global patient safety challenge, following the Clean Care is Safe Care challenge on hand hygiene in 2005 and the Safe Surgery Saves Lives challenge in 2008.
More on the challenge HERE
 COST: Article on preventive and mitigating measures for drug shortages
COST: Article on preventive and mitigating measures for drug shortages
A recent research article published by members of the European Cooperation in Science and Technology (COST) Action 15105 titled ‘Systemic Measures and Legislative and Organizational Frameworks Aimed at Preventing or Mitigating Drug Shortages in 28 European and Western Asian Countries’ signals the need for developing specific definitions of drug shortages, along with methodologies for their monitoring and evaluation. The article points out that the WHO and the European Medicines Agency (EMA) should take the lead in this endeavour, involving pharmaceutical policy researchers and professionals in order to reach an agreed definition, to be used on an international scale.
The article has been produced by members of the COST Action CA 15105 on European Medicines Shortages Research Network—addressing supply problems to patients. COST is the longest-running European framework supporting trans-national cooperation among researchers, engineers and scholars across Europe. COST Actions are bottom-up science and technology networks, open to researchers and stakeholders with a duration of four years. They are active through a range of networking tools, such as workshops, conferences, training schools, short-term scientific missions (STSMs), and dissemination activities.
The report analyses worldwide experiences and studies on medicine shortages, drawing comparisons from case studies and conducting a survey regarding the general characteristics of drug shortages, alertness and information systems linked to drug shortages, public service obligations, and regulations associated with the problem of drug shortages. It presents innovative initiatives and identifies lingering obstacles in addressing supply problems to patients, while encouraging information-sharing and research as the way forward.
Also, the COST Action CA 15105 on European Medicines Shortages Research Network has a new website with information on composition, activities, publications and much more.
Article HERE
New COST Action website HERE
EURORDIS: European Conference on Rare Diseases and Orphan Products
The European Conference on Rare Diseases & Orphan Products (ECRD) is the largest multi-stakeholder gathering in Europe for the rare disease community covering research, development of new treatments, healthcare, social care, public health policies and support at European, national, regional and international levels. ECRD 2018 will take place on 10-12 May 2018, at Messe Wien Congress Center, Vienna, Austria.
“Rare Diseases 360° – collaborative strategies to leave no-one behind” is the overarching theme of ECRD 2018. This theme reinforces the unique quality of this foremost event for the rare disease community in Europe, bringing together and facilitating effective policy discussions between all rare disease stakeholders. It also encompasses the comprehensive range of topic areas covered at the conference and the viewpoint of rare disease patients as equal experts, representing all rare diseases, across borders. Simultaneous interpretation and live streaming of the Opening and Plenary sessions on 11 May 2018 will be available in English, French and German.
The Submission for posters is still open until 12th February 2018. Poster abstracts can be submitted in English and should follow the 9 poster themes outlined. These include: structuring the research & diagnosis landscape; breakthrough medicines on the horizon; the digital patient; quality of life: making what matters, matter; economical perspectives in rare diseases; global rare equity: are we there yet; European Reference Networks; rare diseases patient groups innovations; and open topics.
Poster submission information HERE
More information about ECRD HERE
 EJHP: Junior doctors’ communication with hospital pharmacists about prescribing
EJHP: Junior doctors’ communication with hospital pharmacists about prescribing
The online first edition of the European Journal of Hospital Pharmacy (EJHP) has published an article reporting the findings from a qualitative interview study on Junior doctors’ communication with hospital pharmacists about prescribing. The study interviewed 27 Foundation Year (FY) 1 doctors from three English hospitals, concluding that FY1 doctors and hospital pharmacists communicate frequently about medication prescribing, with less differences in professional judgement than with senior medical staff.
More HERE
--------------------------------------------------------------

Consultations
Commission – Public consultation on pharmaceuticals in the environment
The consultation by the European Commission seeks views on possible actions to address the risks from pharmaceuticals in the environment. Its overall aim is to obtain views and information to support the development of the European Commission's strategic approach to pharmaceuticals in the environment.
Deadline – 21st February 2018
Access survey HERE
Commission – Public consultation on strengthened cooperation against vaccine preventable diseases
Due to the cross-border nature of vaccine preventable diseases and the challenges to national vaccination programmes, the European Commission saw the need to look into common EU actions and an increase of coordination. The information collected via the public consultation is intended to feed into the adoption of a proposal of a Council Recommendation on Strengthened Cooperation against Vaccine Preventable Diseases.
Deadline – 15th March 2018
More information HERE
EMA- Concept paper on the development of a reflection paper on new analytical methods/ technologies in the quality control of herbal medicinal products
Quality control is a prerequisite to assure safe and effective use of (traditional) herbal medicinal products, which are complex mixtures of numerous phytochemical constituents. For the majority of herbal substances, herbal preparations and (traditional) herbal medicinal products the active constituents are not known or are only partly understood. Consequently, EMA is planning to develop a reflection paper that addresses new analytical methods and technologies for the quality control of herbal medicinal products.
Deadline – 30th April 2018
More information HERE
EMA- Draft guideline on safety and efficacy follow-up and risk management of advanced therapy medicinal products
This draft consultation offers the opportunity for proving input regarding the replacement of the 'Guideline on safety and efficacy follow-up - risk management of Advanced Therapy Medicinal Products’, which provides dedicated and specific guidance for ATMPs with regards to the pharmacovigilance system, the identification of risks, the risk minimisation measures, the post-authorisation S&E studies, the management and the reporting of adverse reactions and of the evaluation of the effectiveness of the risk management system.
Deadline – 30th April 2018
More information HERE




