EAHP EU Monitor - 15 April 2014

You can subscribe to receive the EAHP EU Monitor by email here.
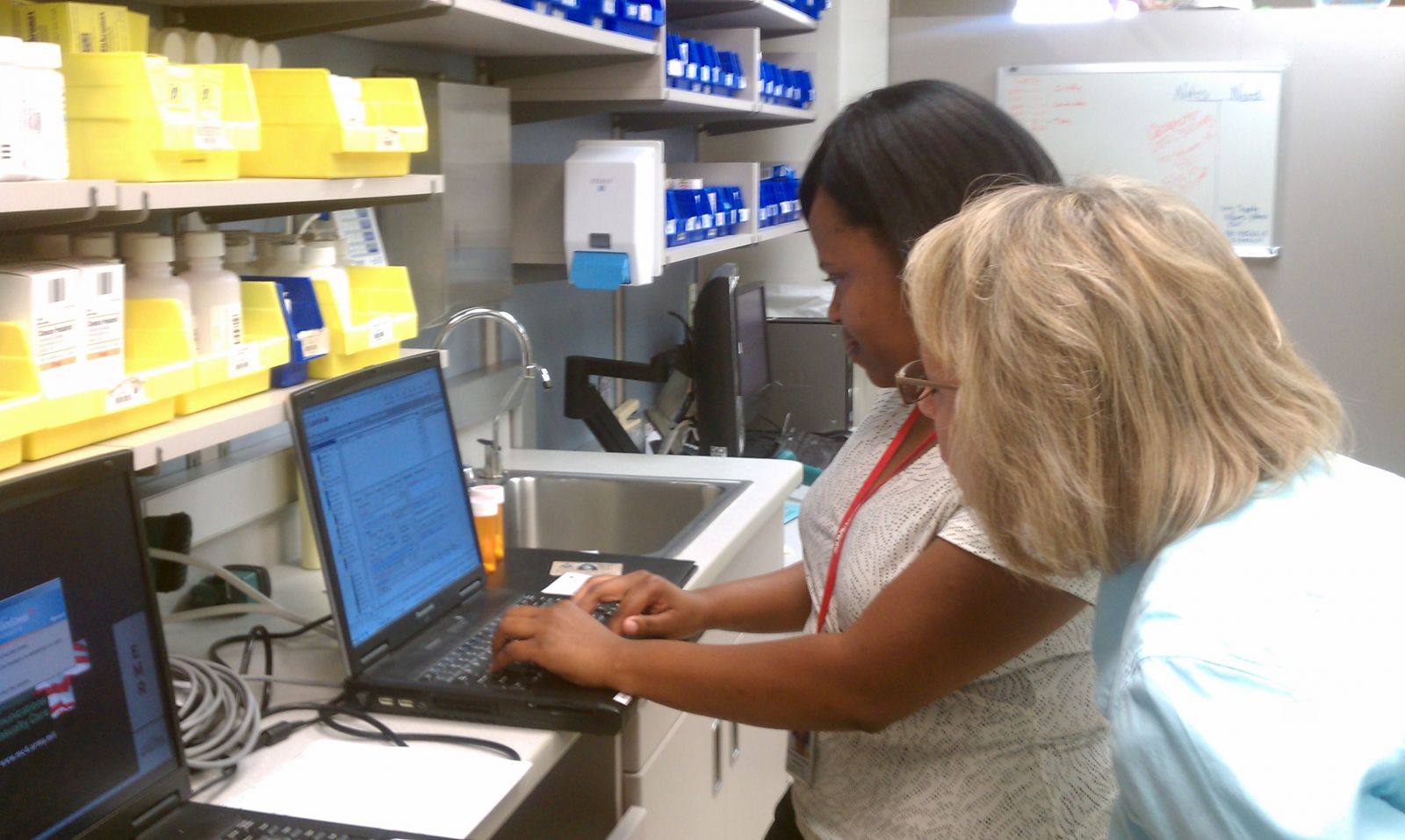
 EAHP 19th Congress looked to the future hospital pharmacist in 2020
EAHP 19th Congress looked to the future hospital pharmacist in 2020
A major talking point of last month’s Congress of the EAHP in Barcelona was the future roles and competencies for hospital pharmacists in the year 2020 and beyond. Drawing from the keynote speech of Dr. Roberto Frontini on Thursday 27th March, attendees debated the extent to which the future hospital pharmacist must more thoroughly adopt ‘social competencies’ in order to effectively communicate with increasingly health literate patients.
More information here.
.png) Clinical Trial results transparency moves to next stage
Clinical Trial results transparency moves to next stage
The European Parliament recently approved, by a large majority (547 in favour and 17 against), plans to overhaul the rules for submitting, assessing and reporting clinical trials across EU Member States.
The new Clinical Trials Regulation stipulates that information from Clinical Study Reports of trials should not generally be considered commercially confidential and will:
- Require that all drug trials in Europe are registered before they begin on the publicly accessible EU clinical trials register.
- Require that a summary of the results from these trials is published on the register within a year of the trial’s end.
- Require that a summary understandable to a lay person of what was found in the trial is published on the register.
- Require Clinical Study Reports (detailed documents normally produced for regulatory processes) to be made publicly available, where they are produced.
- Establish a new publicly accessible EU clinical trials register, to be set up and run by the European Medicines Agency.
- Require that all trials used in support of an application to run a new clinical trial are registered or have published results.
- Impose financial penalties on anyone running a clinical trial who does not adhere to these new laws.
The European Commission has published a useful summary of the new Regulation here.
Shortly after the final vote in the European Parliament on the new regulation, it became know that a court case against the European Medicines Agency on the issue of trial result transparency was dropped. More information here.
 Four reports of eHealth Stakeholder Group published
Four reports of eHealth Stakeholder Group published
On 11 April 2014, the European Commission published a series of reports by the eHealth Stakeholder Group (eHSG), an advisory group of which EAHP was an active member.
The reports related to:
- eHealth interoperability
- patient's access to Electronic Health Records
- eHealth inequalities
- Telemedicine deployment (Key Action 13 of Digital Agenda)
The report on eHealth interoperability is connected to the European Commission’s operational objective, set out in its eHealth Action Plan 2012-2020, to achieve wider interoperability of ehealth services by the end of 2015. The principal recommendations from the stakeholder group to the Commission included:
- focus on priority use cases which have been widely adopted and for which mature specifications exist;
- clarify privacy and data protection requirements; and,
- foster the use of international standards.
On patient access to the electronic health records, the stakeholders recommended that:
- patients should be in charge of their own medical file, and be able to ‘log in’ and inspect it. Amongst the reasoning given was that: “The option to access one‟s own information is a fundamental right that is embodied in the EU Data Protection legislation”;
- access to patients‟ health records should only be permitted to the health professionals directly involved with the patient‟s condition on a need to know basis;
- patients should be given the possibility to know who accessed their EHR and restrict access if they wish so and are informed about the risks of doing so.
The report on ehealth inequalities looked at the concern that the rise of ehealth applications may have an unintended consequence of increasing health inequalities. Stakeholders believed that the speed of change, the costs involved in accessing and upgrading the required hardware/software and devices and various barriers related to insufficient knowledge, skills and literacy, lack of user-friendliness and doubts over the meaningfulness of information can all present the possibility of new health inequalities.
However, if directed appropriately, ehealth could also address inequalities. Sweden is held up in the report as a good case study, with its national strategy on eHealth including provisions on ‘’eServices for accessibility and empowerment’’. Another good case study identified is the practice in Danish hospitals of providing interpretation services via video conferencing, which is particularly useful for migrants unfamiliar with Danish medical culture and treatments.
The report recommends:
- various categories of end users have to be an integral part of the design, evaluation and follow-up during the whole lifecycle of technologies so that particular challenges experienced by specific user groups can be understood and rectified;
- when implementing large-scale eHealth systems, adequate consideration should be given to the needs of vulnerable groups such as children, migrants or people with mental and other disabilities;
- the creation of sufficient incentives for industry to come up with solutions for underserved patients and communities; and,
- some financial subsidies be made available for the purchase of eHealth equipment/ICT access for patients from disadvantaged backgrounds.
The report on telemedicine, advised the Commission to clearly differentiate two types of telemedicine services:
- medical Act type telemedicine services, implying that registered medical doctors perform an existing medical practice over a distance; and,
- telemonitoring type services, services provide multi-professional care teams with physiological parameters of the patient, with the support of remote monitoring technologies
The latter is seen as the more disruptive technology of two, challenging health care organization, professional roles and reimbursement rules. The report’s recommendations include:
- digital literacy and training in using eHealth tools should become part of the educational curricula of all Health Professionals; and,
- benefit and added value of telemedicine services should be systematically monitored and evaluated.
More information about all 4 reports is available here.
EAHP would like to convey its thanks to Leonidas Tzimis and Jacqueline Surugue for their contributions to this work.
 19th Congress of the EAHP: Round-up of media reports
19th Congress of the EAHP: Round-up of media reports
A variety of media reports from the 19th Congress of the EAHP are now available at www.eahp.eu.
From Spanish, UK and Italian media outlets they include interviews with leading EAHP personalities on topical issues and coverage of some of the key seminars on topics such as the future of hospital pharmacy education, and the growing prevalence of medicines shortage problems in Europe.
More information here.
EJHP: Physicochemical compatibility of commonly used analgesics and sedatives in the intensive care medicine
The results of a study into the risk of incompatibilities in parenteral drugs in a cardiovascular intensive care unit have been published in the online first version of the European Journal of Hospital Pharmacy.
The study authors analysed the physical and chemical compatibility of seven commonly used analgesics and sedatives in order to determine whether these drugs can be administered by the same intravenous line.
The seven investigated were: Clonidine hydrochloride, 4-hydroxybutyric acid, (S)-ketamine hydrochloride, lormetazepam, midazolam hydrochloride, piritramide and sufentanil citrate.
More information here.

.gif)



